TB and COVID-19: fighting infectious disease in PNG
Tuberculosis is a disease that has been all-but eradicated in most developed countries. Until the global pandemic, it was the world’s leading cause of death from a single infectious agent; it is now second to COVID-19.
Papua New Guinea has been fighting a tuberculosis (TB) epidemic for many years. In 2018, an estimated 37,000 people had contracted TB with around 4,500 people losing their lives to the disease.
Today, PNG is one of only 14 countries classified as having the triple high burden of tuberculosis, multi-drug resistant tuberculosis and tuberculosis/HIV.
A convergence of infectious disease
In recent weeks, COVID-19 infection rates have soared in PNG.
This health crisis not only threatens to overwhelm the country’s already fragile health system but means access to other health services is now in serious jeopardy.
In both the capital of Port Moresby and in rural areas, many hospitals and clinics are closing wards or turning people away due to a lack of beds, healthcare workers and necessary PPE (personal protective equipment).
Drug sensitive TB typically requires a 6-month treatment program, with patients visiting clinics for review and to obtain drug scripts.
With access to essential health services interrupted, and the government implementing travel restrictions in response to the COVID-19 outbreak, there is a real risk that PNG could see a rise in multi-drug resistant TB.
This more virulent form of the disease requires a long and expensive treatment program. Patients are typically on a drug regime for a 2-year period, with a success rate of only 50%.
According to the Stop TB Partnership, data emerging from India and South Africa shows that people coinfected with TB and COVID-19 have three times higher mortality than people infected with TB alone.
The Partnership warns: “This makes contact tracing, case finding and bi-directional TB and COVID-19 testing essential.”
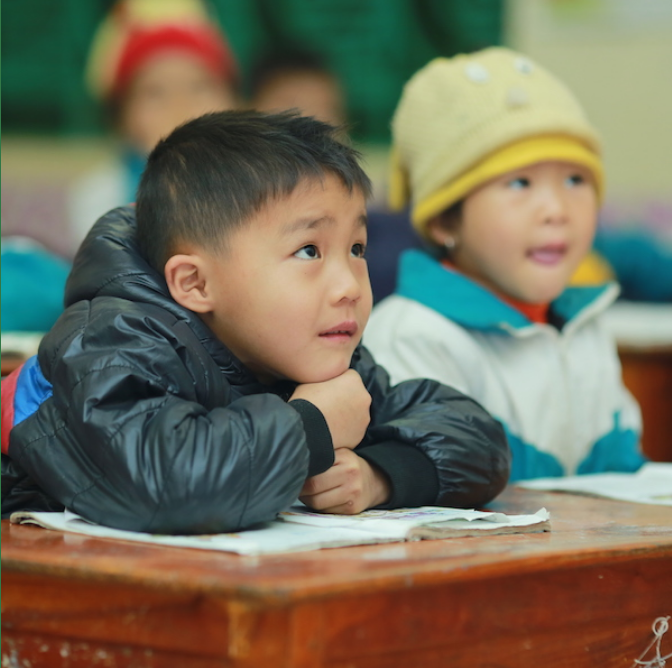
Tuberculosis among PNG’s children
According to data from PNG’s National Department for Health, children account for around one-quarter of detected tuberculosis (TB) cases.
However, paediatric cases of TB can be much more difficult to diagnose, and the disease is frequently overlooked in children.
It can be difficult to get sputum samples from young children, and the disease can be more complex, with children frequently developing extrapulmonary TB, where the infection appears in areas other than the lungs.
According to the World Health Organisation, children are particularly vulnerable to TB meningitis, which has only limited treatment options and a much higher rate of mortality than TB of the lungs.
Causes of PNG’s tuberculosis epidemic
Eradicating TB from Papua New Guinea requires improvements in many sectors of society. Overcrowded housing settlements, a lack of education and poor diets all contribute to the spread of the disease.
Dr Daoni Eserom, the executive manager of public health at the National Department of Health in PNG, notes that poverty creates the conditions in which the disease can flourish. He describes the country’s ongoing battle with TB as a “war”.
Dr Daoni says: “We have a lot of settlements, a lot of unplanned housing and all of these are big contributors to TB.
“Malnutrition, especially in kids, is a very big contributor to TB. So is the ability of households to have the resources to actually seek access to healthcare when they’re sick.”
Access to diagnosis and treatment
To get tested for TB, people must often travel to major urban centres, as small, rural clinics lack testing facilities.
Olive Oa, head of health programs at ChildFund Papua New Guinea, says: “A lack of manpower is one of the biggest issues. In some health centres there are one or two staff, and they are doing everything.”
Patients may have to wait hours if not days to be seen, and this may be after travelling for days to access treatment.
Olive is a fierce and determined participant in the country’s battle to fight the tuberculosis epidemic, and to make sure rural families get diagnosed to begin treatment.
She says: “TB is quite difficult to diagnose in children unless someone is really skilled. The immune system of children is not usually as strong as adults so if you don’t find treatment quickly it can become life threatening.”
By integrating TB education and awareness into maternal and child health programs, Olive says ChildFund can tackle a range of issues that help identify and prevent TB in children: vaccinations, weight checks, dietary information, strategies for avoiding infection, danger signs and disease symptoms, and building general household awareness about what to look for and when to seek treatment.
Olive notes that stigma is also a significant obstacle to TB treatment in PNG. She says: “People should not be afraid of those who are diagnosed with TB. The real danger is from those who are undiagnosed and untreated.”